Laser Optics for Eye Surgery
by Rebecca Charboneau, Edmund Optics
Correcting Refractive Errors
A refractive error is a very common eye disorder where the eye cannot properly focus an image on the retina, or focal point, at the back of the eye (Figure 1). Common types of refractive errors include myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. There are more than 88.4 million people that have a refractive error resulting in blurred vision.1 Fortunately, modern technology has allowed for the invention of laser eye surgery to correct refractive errors. The optically transparent structures of the eye allow for the delivery of a laser beam from ultraviolet (UV) to near infrared (NIR) wavelengths to noninvasively alter ophthalmic tissue.2

Figure 1: Common refractive errors
The most common form of laser eye surgery to correct vision is laser-assisted in situ keratomileusis, commonly referred to as LASIK. LASIK involves using an excimer laser to reshape the eye’s cornea to correct for common refractive errors. Excimer lasers are pulsed gas lasers that emit UV light through the stimulated emission of the gas molecules, like F2 or ArF, within the laser cavity. The excimer laser is able to ablate layers of the cornea that are microns thick to reshape the cornea and correct for refractive errors.
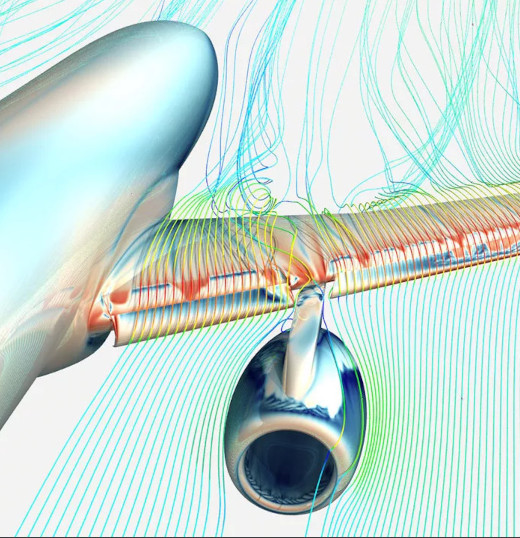
Figure 2 shows an optical path of a LASIK surgical device that utilizes an excimer laser and a femtosecond laser for correcting refractive errors. For the ultrafast laser, a fiber-coupled source with pulse durations between 100-800 fs and wavelength of 1064 nm is typical for LASIK devices. The ultrafast beam first passes through a transmission grating to compress the stretched pulse to ensure peak power is maintained. Then the beam is reflected into a beam expander before being sent through an F-theta lens for focusing onto a patient’s eye to create the cornea flap. Once the flap is created, the excimer laser is delivered to the patient’s eye by first being reflected off a mirror through a homogenizer, which can be a flat top laser beam shaper. The homogenizer modifies the beam to maintain consistent optical intensity before passing through a beam shaping assembly. A dichroic filter is used to then reflect the UV excimer beam through a focusing lens to ablate the cornea.

Figure 2: LASIK optical path
Treating Cataract and Glaucoma
The most prevalent ocular disease and major cause of blindness in the world is cataract.3 Impaired vision from cataract is caused by protein clumps or discolored pigment that are deposited in the lens of the eye, reducing the transmission of light to the retina (Figure 3). Cataract is treated effectively through surgical laser procedures that are used to replace the clouded lenses with an artificial intraocular lens (IOL). In order to replace the lens, the existing lens must be fragmented and removed to make space for the IOL implant. Lens fragmentation can be accomplished by an ultrafast laser that precisely controls the output power and beam delivery to safely break up the clouded lens.

Figure 3: Cataract symptoms
Common femtosecond lasers used in cataract surgical devices are solid-state lasers such as neodymium-doped yttrium aluminum garnet (Nd:YAG), erbium-doped YAG (Er:YAG), or titanium-sapphire (Ti:Sapphire) lasers. In order to accurately control the power of ultrafast laser pulses, the laser needs to be coupled with precise, fast-deflecting, focusing optics which are guided by imaging systems that use optical coherence tomography (OCT). Figure 4 below demonstrates the optical path of a cataract surgical device that uses a Ti:Sapphire femtosecond laser. The ultrafast laser has a typical pulse length of 100fs to 1000fs and potential wavelengths of ~800nm, 1030nm, or 1064nm depending on the source. The beam passes through a scanning lens system that contains aspheric elements to reduce spherical aberration and maintain beam quality. After propagation through galvanometric mirrors for deflection, the laser passes through a beamsplitter where a portion of the light is directed to the OCT system for beam positioning. Aspheres are used to concentrate the beam for lens fragmentation. Compared to a LASIK device, the diameter of the laser focus spot is larger for cataract surgery to provide adequate photodysruption.4

Figure 4: Cataract laser surgical device optical path
Another ocular disease that can be treated with a similar system is glaucoma. Glaucoma is a degenerative disease that damages the optic nerve through the loss of retinal ganglion cells.5 As ganglion cells are damaged, gradual vision loss occurs as communication to the optic nerve is cut off.5 Selective laser trabeculoplasty (SLT) is the preferred treatment for glaucoma; SLT uses a 532nm frequency-doubled Nd:YAG laser to deliver nanosecond pulses to widen drainage channels in the trabecular meshwork for eye pressure relief. A notable variation to the optical path of an SLT system is the use of nonlinear crystals to generate 532nm from a 1064nm laser source. This method is preferred compared to using just a 532nm source because it stabilizes the energy of each laser pulse to ensure minimal damage to adjacent retinal tissue.6
Treating Diabetic Retinopathy
Laser eye surgery is also used to treat diabetic retinopathy. This disease is induced by high blood sugar levels that cause damage to blood vessels in the retina.7 Retinal damage is caused by swelling or leaky blood vessels and, as a result, can cause vision loss (Figure 5). Laser photocoagulation is the first-line therapy for treating diabetic retinopathy to prevent the formation of unwanted blood vessels and shrink any leaking vessels. Visible (VIS) or NIR wavelength gas, diode, dye, and YAG lasers are used in laser photocoagulation. Unlike LASIK and cataract surgical lasers, ultrafast lasers are not typically used for photocoagulation. Nanosecond pulsed or modulated CW lasers with a duty cycle anywhere from 10-100ms are often the desirable choice as they induce blood vessel clotting without permanent damage to nearby tissue.8 Collimating and cylindrical lenses are commonly used in a laser photocoagulation system to propagate and shape the beam to be focused on the retina. Laser photocoagulation can also be combined with a vitrectomy, which is a treatment that removes fluid called the vitreous that has been clouded by leaky blood vessels.7

Figure 5: Diabetic retinopathy symptoms
Look into the Future
Advanced ophthalmic technologies are in increasing demand due to changing lifestyles, aging, and population growth. There is a need for faster and more effective laser treatments that will allow ophthalmologists to treat more patients. Direct selective laser trabeculoplasty (DSLT) is a new laser treatment for glaucoma that directly delivers the laser beam without gonioscopy.9 DSLT has proven to be a more efficient treatment as it uses automated image acquisition and eye tracking algorithms to deliver the beam to the trabecular meshwork.9 Another recent advancement is small incision lenticule extraction (SMILE) which is an alternative to LASIK. SMILE requires only a small incision in the cornea as opposed to the flap that LASIK requires. This significantly improves patient recovery time and comfort during surgery, making it an attractive option for correcting refractive errors.10
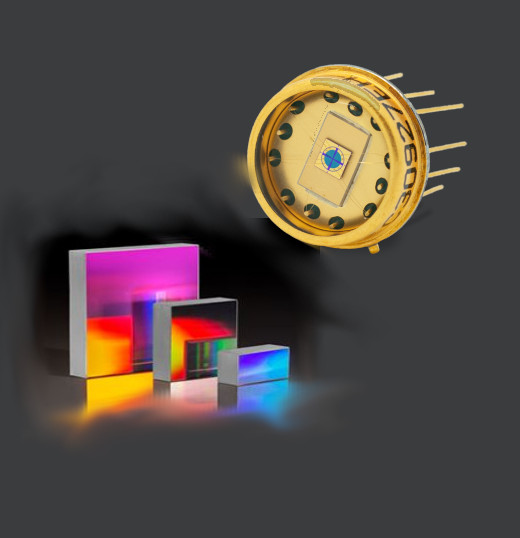
Edmund Optics® is committed to expanding our product selection to support advances in ophthalmic surgery technology. Edmund Optics® has in-house manufacturing of laser optics components, fully-custom design capabilities, and state-of-the-art metrology to meet customer specifications. Our extensive knowledge around laser optics makes Edmund Optics® a trusted partner for the development of ophthalmic technologies to make treatments more accessible and effective.
References
- World Health Organization. (2021 October 14). Blindness and vision impairment. World Health Organization.
- Thomas Asshauer, Catharina Latz, Alireza Mirshahi, and Christian Rathjen. (2021 November 25). Femtosecond lasers for eye surgery applications: historical overview and modern low pulse energy concepts. Advanced Optical Technologies.
- Hui Sun, Andreas Fritz, Gerit Dröge, Tobias Neuhann, and Josef F. Bille. (2019 August 14). High resolution imaging in microscopy and ophthalmology: new frontiers in biomedical optics. National Library of Medicine.
- Jorge L. Alió. (2011 July). Cataract surgery with femtosecond lasers. Saudi Journal of Ophthalmology, 25(3): 219-223.
- Karen Allison, Deepkumar Patel, and Omobolanle Alabi. (2022 November). Epidemiology of glaucoma: the past, present, and predications for the future. Cureus, 12(11).
- A. Garg and G. Gazzard. (2018 May). Selective laser trabeculoplasty: past, present, and future. Eye, 32(5): 863-876.
- Ninel Z. Gregori. (2021 September 14). Diabetic retinopathy: causes, symptoms, treatment. American Academy of Ophthalmology.
- Samuel H. Yun and Ron A. Adelman. (2015 April-June). Recent developments in laser treatment of diabetic retinopathy. Middle East African Journal of Ophthalmology, 22(2): 157-163.
- Mordechai Goldenfeld, Michael Belkin, Masha Dobkin-Bekman, Zachary Sacks, Sharon Blum Meirovitch, Noa Geffen, Ari Leshno, and Alon Skaat. (2021 March). Automated direct selective laser trabeculoplasty: first prospective clinical trial. Translational Vision Science & Technology, 10(3): 5.
- Kathryn Hatch. (2020 May 14). Small incision lenticule extraction (SMILE): it’s what’s new in laser vision correction. Harvard Health Publishing.
Heard on the Internet
Imagination is more important than knowledge.
Albert Einstein